AMOR-IPAT
Early Term Issues
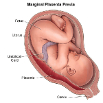
Multiple institutions (ACOG, March of Dimes, the Joint Commission) have published opinions and clinical guidelines stating that early-term, non-indicated labor induction leads to increased rates of neonatal morbidity. As a result, non-indicated labor induction prior to 39 weeks 0 days of gestation is no longer possible in many parts of the USA. However, the use of early-term, non-indicated labor induction has only been studied in retrospective format and the data so produced – while statistically significant – may be heavily confounded (confounded by indication). Published data to date do not contain enough strength (e.g., relative risk values greater than 3) to be conclusive. Randomized clinical trials are needed to compare the outcomes of early-term, non-indicated labor induction to the outcomes of expectant management beyond the early-term period. This is especially important because several studies have suggested that restricting the use of early-term labor induction might increase the risk of one of the worst birth outcomes, i.e., early-term stillbirth. Specifically, it is well known that the cumulative risk of term stillbirth increases as a function of increasing gestational age. Hence, a new policy that limits early-term labor induction will necessarily push some pregnancies longer into the term period, and this will necessarily increase the incidence of term stillbirth. It is unfortunate that a major effort has been used to restrict the use of early-term labor induction in the absence of a high-quality research foundation, and it is even more unfortunate that the restriction of early-term, non-indicated labor induction may be directly responsible for increasing the incidence of early term stillbirth in this country.
Many people are of the opinion that babies “know when to come” and that labor should not be started artificially without an accepted ACOG indication. However, term stillbirth occurs with a rate of about 1 episode per 1000 births. This fact alone requires that we question the basis of the statement babies “know when to come”. Is this a medical fact, or is it just a dearly held belief?
Randomized clinical trials of early-term labor induction are needed to see if the AMOR-IPAT approach improves, does not change, or worsens rates of important adverse birth outcomes. A recent meta-analysis of RCTs concluded that non-indicated labor induction, as compared to expectant management, improves birth outcomes. If early-term risk-based “non-indicated” labor induction improves, or does not worsen, rates of adverse birth outcomes, and if early-term risk-based “non-indicated” labor induction decreases the risk of early-term intra-uterine fetal demise (i.e., IUFD, or stillbirth), then perhaps the use of early-term risk-based labor induction should be discussed with patients as an option for care at 37 weeks of gestation.